Singapore Healthcare Claims Management Market Analysis
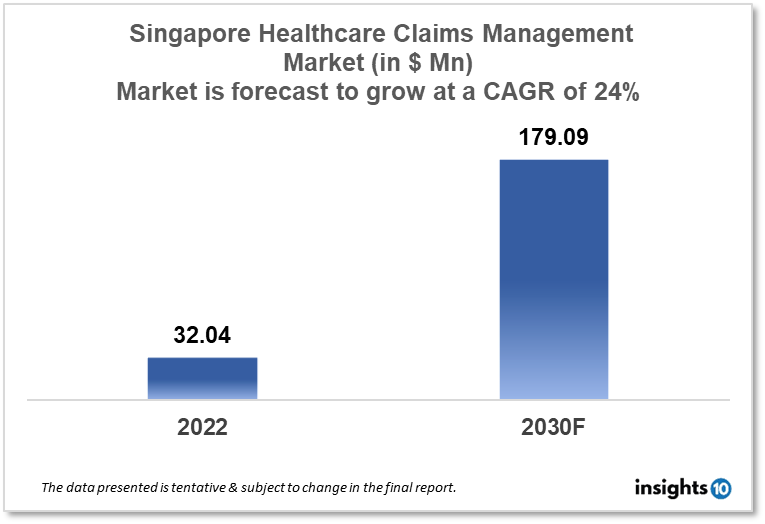
The Singapore healthcare claims management market is projected to grow from $32.04 Mn in 2022 to $179.09 Mn by 2030, registering a CAGR of 24% during the forecast period of 2022 - 2030. The main factors driving the growth would be growing awareness, technological advancements and government initiatives. The market is segmented by component, type, by delivery mode and end-user. Some of the major players include Fullerton Health, Igloo, Fermion, Accenture and Optum.
Buy Now

Singapore Healthcare Claims Management Market Executive Summary
The Singapore healthcare claims management market is projected to grow from $32.04 Mn in 2022 to $179.09 Mn by 2030, registering a CAGR of 24% during the forecast period of 2022 - 2030. Singapore spent $2,633 on healthcare per person in 2019, a decrease of 1.31% from the year before. It only spent 4.09% of its GDP on healthcare, which was relatively low compared to many other industrialised nations.
The healthcare system in Singapore is among the best in the world, with a strong emphasis on quality, accessibility, and affordability. A wide variety of public and private healthcare providers, including hospitals, clinics, and medical facilities, support the nation's healthcare sector.
Healthcare claims management, which entails the processing and payment of medical claims by insurance companies, is a crucial component of the healthcare sector. Due to the increased demand for healthcare services and the growing volume of insurance claims, Singapore's healthcare claims management market is expanding. Healthcare claims management businesses in Singapore are using technology to accelerate the processing and settlement of claims in order to meet this growing demand. These businesses are implementing cutting-edge automation and analytics solutions to increase the speed and accuracy of claims processing, which also lowers costs and enhances the overall client experience.
Market Dynamics
Market Growth Drivers
The Singapore healthcare claims management market is expected to be driven by factors such as:
- Growing awareness- People in Singapore are becoming more aware of the value of healthcare and the requirement for health insurance as a result of the increased availability of information and services. As a result, there are more health insurance plans on the market, which has increased demand for healthcare claims management services
- Technological advancements- To increase the speed and accuracy of claims processing, healthcare claims management organisations in Singapore are implementing cutting-edge technology like artificial intelligence, machine learning, and blockchain
- Government initiatives- The Singaporean government has launched a number of measures to promote the use of health insurance and raise the standard of medical care. The demand for healthcare claims management services has increased as a result of these efforts increased enrolment in health insurance coverage
Market Restraints
The following factors are expected to limit the growth of the healthcare claims management market in Singapore:
- Regulatory constraints- Healthcare claims management organisations must comply with stringent rules and regulations due to the intense regulation of the healthcare sector in Singapore. This can restrict these businesses' capacity for innovation and the development of new technologies, which might have an effect on the market's expansion
- Limited insurance coverage- Despite an increase in the number of Singaporeans purchasing health insurance plans, a sizable portion of the population remains uninsured. This restricts the size of the possible market for healthcare claims management companies and may hinder their ability to expand
- Cost pressures- Healthcare claims management firms must control costs to stay competitive, yet there are cost constraints in the market, such as increasing labour costs and the requirement to invest in new technologies. Healthcare claims management firms' profitability and capacity to finance expansion plans may be impacted by these cost pressures
Competitive Landscape
Key Players
- Fullerton Health (SGP)- provides clinics and facilities within the healthcare network with affordable administration and management solutions. They provide services including processing insurance claims and providing emergency medical care. Their technological infrastructure enables them to perform more than only management and administration of crucial functions for healthcare providers. They evaluate and assess the market through data mining and analysis to provide data that could assist healthcare providers cut costs and being more prepared
- Igloo (SGP)- an internet platform for health and property and casualty insurance. It provides coverage for several insurance types, such as content insurance, social insurance, health insurance, and more. For the benefit of the policyholders, it has a platform for claims administration. It also provides AI-based software for a variety of tasks, including claim processing, sales & distribution, market development, and more
- Fermion (SGP)- an insurance startup that provides solutions for the insurance industry's product development and policy claims on the cloud. It offers complete digital transformation solutions that empower financial service companies, insurers, and more
- Accenture- a global professional services company that provides consulting, technology, and outsourcing services to clients in Singapore and everywhere else in the world, including options for managing medical claim payments
- Optum- is committed to making healthcare delivery better, creating opportunities for clients to have better experiences, better health, and lower costs
Notable Upcoming Events
May 2023- The 18th Asia conference on healthcare and health insurance is scheduled on 10-11 May 2023 in Singapore. The Theme of this conference is "Reimagining Health Insurance: addressing pain points towards a promising future!"
1. Executive Summary
1.1 Service Overview
1.2 Global Scenario
1.3 Country Overview
1.4 Healthcare Scenario in Country
1.5 Healthcare Services Market in Country
1.6 Recent Developments in the Country
2. Market Size and Forecasting
2.1 Market Size (With Excel and Methodology)
2.2 Market Segmentation (Check all Segments in Segmentation Section)
3. Market Dynamics
3.1 Market Drivers
3.2 Market Restraints
4. Competitive Landscape
4.1 Major Market Share
4.2 Key Company Profile (Check all Companies in the Summary Section)
4.2.1 Company
4.2.1.1 Overview
4.2.1.2 Product Applications and Services
4.2.1.3 Recent Developments
4.2.1.4 Partnerships Ecosystem
4.2.1.5 Financials (Based on Availability)
5. Reimbursement Scenario
5.1 Reimbursement Regulation
5.2 Reimbursement Process for Services
5.3 Reimbursement Process for Treatment
6. Methodology and Scope
Healthcare Claims Management Market Segmentation
By Component (Revenue, USD Billion):
Further breakdown of the software and services segment of the healthcare claims management market
- Software
- Services
By Type (Revenue, USD Billion):
Although they have nothing to do with it, skills unrelated to patient care are equally crucial for any healthcare organization that wants to stay in business. Among these are managing intricate insurance regulations, comprehending best practices for data collection, and analyzing data to identify areas for development. For the above reasons, providers are constantly looking for methods to improve claim administration and medical billing systems. Setting up an integrated billing and claims processing system is one approach to accomplish this, which has a number of benefits.
- Integrated Solutions
- Standalone Solutions
By Delivery Mode (Revenue, USD Billion):
- On-Premise
- Cloud-Based
By End User (Revenue, USD Billion):
- Healthcare Payers
- Healthcare Providers
- Other End Users
Healthcare payers in this market are anticipated to rise quickly over the course of the projection period because of the installation of strict regulatory requirements, a lack of experienced personnel internally for claims processing, rising healthcare expenditures, and fraud associated with those charges. Payers have also assisted healthcare providers by creating a web-based and cloud-based interface that helps them manage medical billing and associated claims and offers accurate and timely information about the epidemic.
Methodology for Database Creation
Our database offers a comprehensive list of healthcare centers, meticulously curated to provide detailed information on a wide range of specialties and services. It includes top-tier hospitals, clinics, and diagnostic facilities across 30 countries and 24 specialties, ensuring users can find the healthcare services they need.
Additionally, we provide a comprehensive list of Key Opinion Leaders (KOLs) based on your requirements. Our curated list captures various crucial aspects of the KOLs, offering more than just general information. Whether you're looking to boost brand awareness, drive engagement, or launch a new product, our extensive list of KOLs ensures you have the right experts by your side. Covering 30 countries and 36 specialties, our database guarantees access to the best KOLs in the healthcare industry, supporting strategic decisions and enhancing your initiatives.
How Do We Get It?
Our database is created and maintained through a combination of secondary and primary research methodologies.
1. Secondary Research
With many years of experience in the healthcare field, we have our own rich proprietary data from various past projects. This historical data serves as the foundation for our database. Our continuous process of gathering data involves:
- Analyzing historical proprietary data collected from multiple projects.
- Regularly updating our existing data sets with new findings and trends.
- Ensuring data consistency and accuracy through rigorous validation processes.
With extensive experience in the field, we have developed a proprietary GenAI-based technology that is uniquely tailored to our organization. This advanced technology enables us to scan a wide array of relevant information sources across the internet. Our data-gathering process includes:
- Searching through academic conferences, published research, citations, and social media platforms
- Collecting and compiling diverse data to build a comprehensive and detailed database
- Continuously updating our database with new information to ensure its relevance and accuracy
2. Primary Research
To complement and validate our secondary data, we engage in primary research through local tie-ups and partnerships. This process involves:
- Collaborating with local healthcare providers, hospitals, and clinics to gather real-time data.
- Conducting surveys, interviews, and field studies to collect fresh data directly from the source.
- Continuously refreshing our database to ensure that the information remains current and reliable.
- Validating secondary data through cross-referencing with primary data to ensure accuracy and relevance.
Combining Secondary and Primary Research
By integrating both secondary and primary research methodologies, we ensure that our database is comprehensive, accurate, and up-to-date. The combined process involves:
- Merging historical data from secondary research with real-time data from primary research.
- Conducting thorough data validation and cleansing to remove inconsistencies and errors.
- Organizing data into a structured format that is easily accessible and usable for various applications.
- Continuously monitoring and updating the database to reflect the latest developments and trends in the healthcare field.
Through this meticulous process, we create a final database tailored to each region and domain within the healthcare industry. This approach ensures that our clients receive reliable and relevant data, empowering them to make informed decisions and drive innovation in their respective fields.
To request a free sample copy of this report, please complete the form below.
We value your inquiry and offer free customization with every report to fulfil your exact research needs.









































