Egypt Healthcare Claims Management Market Analysis
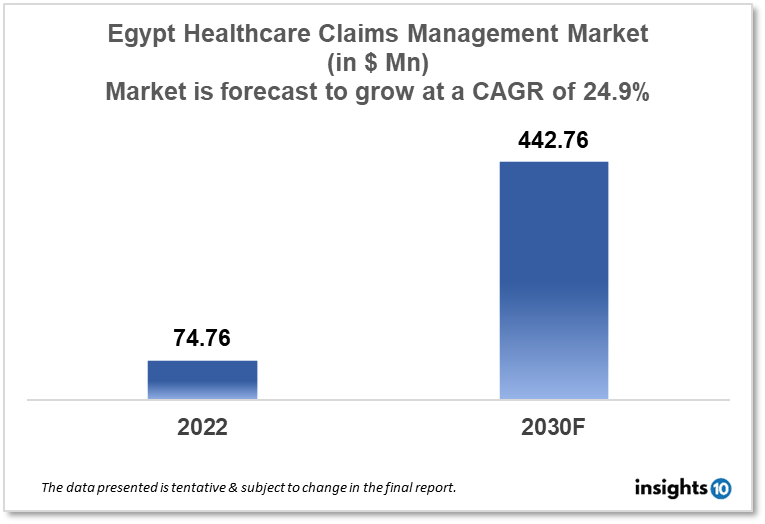
Egypt's healthcare claims management market is projected to grow from $74.76 Mn in 2022 to $442.76 Mn by 2030, registering a CAGR of 24.9% during the forecast period of 2022-30. The main factors driving the growth would be rising health insurance coverage, increasing patient awareness and expectations, government initiatives, and growing demand for digital healthcare technology. The market is segmented by component, type, delivery mode, and by end-user. Some of the major players include MedMisr, Marsh, Cigna, Allianz and Accenture.
Buy Now

Egypt Healthcare Claims Management Market Executive Summary
Egypt's healthcare claims management market is projected to grow from $74.76 Mn in 2022 to $442.76 Mn by 2030, registering a CAGR of 24.9% during the forecast period of 2022-30. Egypt's healthcare industry cost 4.74% of GDP, or $150 per person, in 2019. The improvement of healthcare and population health is a top priority for the Egyptian government in line with the Sustainable Development Goals (SDGs) of the UN.
Healthcare entrepreneurs are discovering previously unthinkable opportunities to make a mark and create a brighter tomorrow as a result of the long-standing social and economic issues that developing nations like Egypt are pursuing to provide higher-quality healthcare services.
Due to the increased demand for healthcare services, rising healthcare expenses, and the requirement for efficient and effective management of healthcare claims, the market for healthcare claims management in Egypt has been expanding quickly. In Egypt, there is pressure on healthcare providers and insurance companies to save costs while still providing high-quality care, which has increased the need for creative solutions to simplify the claims handling process.
Market Dynamics
Market Growth Drivers
The Egypt healthcare claims management market is expected to be driven by factors such as:
- Rising health insurance coverage- Egypt has been increasing the number of people who are covered by the government's national health insurance program. As a result, there are now more medical claims being filed, which has increased the demand for effective claims management solutions
- Increasing patient awareness and expectations- People in Egypt are expecting higher-quality healthcare services as they become more aware of their rights. This has heightened the need for prompt reimbursements and transparency in the claims management process, both of which may be met by effective claims management solutions
- Government initiatives- The Egyptian government is putting more of an emphasis on expanding health insurance coverage, enhancing healthcare infrastructure and services, and promoting the use of digital healthcare technologies. These activities are anticipated to foster an environment that would support the expansion of Egypt's healthcare claims management sector
- Growing demand for digital healthcare technology- Egypt is increasingly using digital healthcare technology like EHRs, telemedicine, and mHealth solutions. Healthcare claims administration is predicted to become more accurate and efficient thanks to these technologies, which will raise demand for claims management software
Market Restraints
The following factors are expected to limit the growth of the healthcare claims management market in Egypt:
- Limited technology infrastructure- The lack of adequate technical infrastructure in Egypt, particularly in the healthcare industry, is one of the major impediments. Healthcare providers and insurance firms may find it challenging to process claims and manage their data effectively as a result
- Limited regulatory oversight- Inconsistencies and fraud may result from the current lack of regulatory monitoring of Egypt's market for healthcare claims management
- Limited health insurance coverage- The entire size of the healthcare claims management market may be constrained by the low rate of health insurance coverage in Egypt
Competitive Landscape
Key Players
- MedMisr (EGY)- is the first digital healthcare benefits management system in Egypt. With an innovative real-time, paperless, and secure platform for claim management that begins at the first point of service, MEDMISR is focused on replacing the old claims form procedure with a digital document. It provides a cost-optimization solution for medical insurance. By removing the traditional claim form, delivering a cost optimization solution with an entirely new user experience, linking all stakeholders online, and enabling fraud protection, MedMisr seeks to transform the medical insurance industry
- Cigna- an international health services company which provides health insurance and related services in China. The company offers several services for managing healthcare claims, such as provider network management, customer support, and claims processing
- Allianz- a one-stop shop for all needs relating to life and health insurance. It offers alternatives for short-term or emergency protection, critical illness, life and disability insurance, and foreign health insurance
- Accenture- a global professional services company that provides healthcare claims administration services to clients in Italy and other countries. Accenture's healthcare management services include customer assistance, fraud and abuse detection, analytics and reporting, and claims processing and management
1. Executive Summary
1.1 Service Overview
1.2 Global Scenario
1.3 Country Overview
1.4 Healthcare Scenario in Country
1.5 Healthcare Services Market in Country
1.6 Recent Developments in the Country
2. Market Size and Forecasting
2.1 Market Size (With Excel and Methodology)
2.2 Market Segmentation (Check all Segments in Segmentation Section)
3. Market Dynamics
3.1 Market Drivers
3.2 Market Restraints
4. Competitive Landscape
4.1 Major Market Share
4.2 Key Company Profile (Check all Companies in the Summary Section)
4.2.1 Company
4.2.1.1 Overview
4.2.1.2 Product Applications and Services
4.2.1.3 Recent Developments
4.2.1.4 Partnerships Ecosystem
4.2.1.5 Financials (Based on Availability)
5. Reimbursement Scenario
5.1 Reimbursement Regulation
5.2 Reimbursement Process for Services
5.3 Reimbursement Process for Treatment
6. Methodology and Scope
Healthcare Claims Management Market Segmentation
By Component (Revenue, USD Billion):
Further breakdown of the software and services segment of the healthcare claims management market
- Software
- Services
By Type (Revenue, USD Billion):
Although they have nothing to do with it, skills unrelated to patient care are equally crucial for any healthcare organization that wants to stay in business. Among these are managing intricate insurance regulations, comprehending best practices for data collection, and analyzing data to identify areas for development. For the above reasons, providers are constantly looking for methods to improve claim administration and medical billing systems. Setting up an integrated billing and claims processing system is one approach to accomplish this, which has a number of benefits.
- Integrated Solutions
- Standalone Solutions
By Delivery Mode (Revenue, USD Billion):
- On-Premise
- Cloud-Based
By End User (Revenue, USD Billion):
- Healthcare Payers
- Healthcare Providers
- Other End Users
Healthcare payers in this market are anticipated to rise quickly over the course of the projection period because of the installation of strict regulatory requirements, a lack of experienced personnel internally for claims processing, rising healthcare expenditures, and fraud associated with those charges. Payers have also assisted healthcare providers by creating a web-based and cloud-based interface that helps them manage medical billing and associated claims and offers accurate and timely information about the epidemic.
Methodology for Database Creation
Our database offers a comprehensive list of healthcare centers, meticulously curated to provide detailed information on a wide range of specialties and services. It includes top-tier hospitals, clinics, and diagnostic facilities across 30 countries and 24 specialties, ensuring users can find the healthcare services they need.
Additionally, we provide a comprehensive list of Key Opinion Leaders (KOLs) based on your requirements. Our curated list captures various crucial aspects of the KOLs, offering more than just general information. Whether you're looking to boost brand awareness, drive engagement, or launch a new product, our extensive list of KOLs ensures you have the right experts by your side. Covering 30 countries and 36 specialties, our database guarantees access to the best KOLs in the healthcare industry, supporting strategic decisions and enhancing your initiatives.
How Do We Get It?
Our database is created and maintained through a combination of secondary and primary research methodologies.
1. Secondary Research
With many years of experience in the healthcare field, we have our own rich proprietary data from various past projects. This historical data serves as the foundation for our database. Our continuous process of gathering data involves:
- Analyzing historical proprietary data collected from multiple projects.
- Regularly updating our existing data sets with new findings and trends.
- Ensuring data consistency and accuracy through rigorous validation processes.
With extensive experience in the field, we have developed a proprietary GenAI-based technology that is uniquely tailored to our organization. This advanced technology enables us to scan a wide array of relevant information sources across the internet. Our data-gathering process includes:
- Searching through academic conferences, published research, citations, and social media platforms
- Collecting and compiling diverse data to build a comprehensive and detailed database
- Continuously updating our database with new information to ensure its relevance and accuracy
2. Primary Research
To complement and validate our secondary data, we engage in primary research through local tie-ups and partnerships. This process involves:
- Collaborating with local healthcare providers, hospitals, and clinics to gather real-time data.
- Conducting surveys, interviews, and field studies to collect fresh data directly from the source.
- Continuously refreshing our database to ensure that the information remains current and reliable.
- Validating secondary data through cross-referencing with primary data to ensure accuracy and relevance.
Combining Secondary and Primary Research
By integrating both secondary and primary research methodologies, we ensure that our database is comprehensive, accurate, and up-to-date. The combined process involves:
- Merging historical data from secondary research with real-time data from primary research.
- Conducting thorough data validation and cleansing to remove inconsistencies and errors.
- Organizing data into a structured format that is easily accessible and usable for various applications.
- Continuously monitoring and updating the database to reflect the latest developments and trends in the healthcare field.
Through this meticulous process, we create a final database tailored to each region and domain within the healthcare industry. This approach ensures that our clients receive reliable and relevant data, empowering them to make informed decisions and drive innovation in their respective fields.
To request a free sample copy of this report, please complete the form below.
We value your inquiry and offer free customization with every report to fulfil your exact research needs.