China Financial Assistance Programs Market Analysis
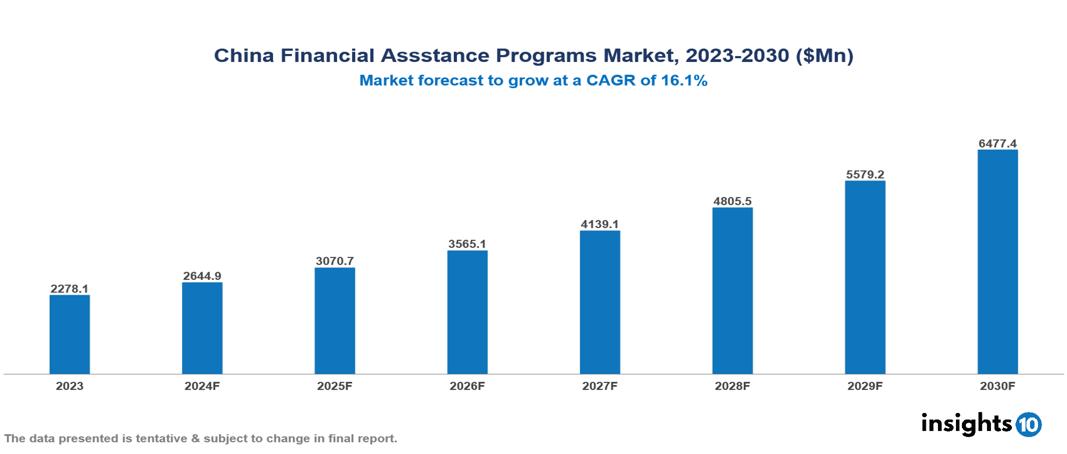
The China Financial Assistance Programs Market was valued at $2,278.1 Mn in 2023 and is projected to grow at a CAGR of 16.1% from 2023 to 2023, to $6,477.4 Mn by 2030. The market is driven by various sector such as rising drug cost, complex insurance landscape, regulatory environment, market competition, patient adherence concern etc. The prominent pharmaceutical companies providing financial assistance to patient are such as CSPC Pharmaceuticals, Cardinal Health, Sinopharm Group Co Ltd, Merck, GSK, Johnson & Johnson, Novartis among others.
Buy Now

China Financial Assistance Programs Market Executive Summary
The China Financial Assistance Programs Market is at around $2,278.1 Mn in 2023 and is projected to reach $6,477.4 Mn in 2030, exhibiting a CAGR of 16.1% during the forecast period 2023-2030.
Patients' out-of-pocket drug cost sharing is determined by their health plans or pharmacy benefit manager's (PBM's) formulary--a list of preferred and nonpreferred prescription drugs. Preferred status is based on a drug's effectiveness, price, and the level of rebate the payer receives from the manufacturer for giving the drug preference over its competitors. Generics and preferred brand drugs are generally assigned lower patient cost sharing than nonpreferred brand drugs. As drug prices have increased, so has patient cost sharing, causing some patients to stretch, forgo, or discontinue medication that is too expensive. Drug manufacturers often seek to mitigate these effects by providing or funding various forms of patient financial support. The aim of drug manufacturers' patient financial support is to minimize or remove out-of-pocket cost sharing as an obstacle when patients choose medications, thereby keeping them on brand-name drugs for longer.
There is an increasing prevalence of chronic diseases in China, in 2022, there were around 197 deaths in China from major cardiovascular diseases per 100,000 population and 3.7 Mn people were living with diagnosed diabetes out of which 10.1% were males and 8.7% were females. Therefore, the market is predominately driven by factors such as chronic disease prevalence, and aging demographic whereas reimbursement challenges, lack of awareness and budgetary pressures restrict market growth.
Pharmaceutical companies providing financial assistance to patient are such as Merck, GSK, Pfizer, Johnson & Johnson, Novartis among others.
Market Dynamics
Market Drivers
Chronic disease prevalence: The national prevalence of any chronic diseases was 81.1% among Chinese adults. The growing number of patients requiring long-term, frequently costly therapies is due to chronic illnesses. This results in a long-term, ongoing demand for financial help. The treatment of chronic illnesses is a top concern in medicine, which motivates support for aid initiatives.
Rising population of people aged above 65: The aging population in China is increasing at a rate of 28%, will reach o population of 408 Mn by 2024, this is making them more prone to diseases requiring long time treatment and are more inclined towards help from pharmaceuticals and medications thus it is boosting the market of financial assistance in China.
Market Restraints
Reimbursement Challenges: Reimbursement challenges and limited coverage of financial assistance services under Saudi Arabia's healthcare system also pose barriers to wider adoption. Thus, limiting its accessibility and growth.
Lack of awareness: Lack of awareness and understanding about the benefits of financial assistance programs among both patients and healthcare providers in Saudi Arabia is a key challenge. Limiting the adoption financial assistance and ultimately limiting its growth.
Budgetary pressures: Pharmaceutical companies must balance the cost of assistance programs with maintaining profit margins. Economic downturns or changes in company strategy could lead to reduced funding for these programs. This pressure might result in more selective or limited assistance offerings.
Regulatory Landscape and Reimbursement Scenario
China's reimbursement mechanism significantly impacts the pricing of pharmaceutical products. The National Reimbursable Drug List (NRDL) is a key component, as it determines which drugs are eligible for reimbursement by the Basic Medical Insurance (BMI) scheme. Once a drug is included on the NRDL, the National Healthcare Security Administration (NHSA) negotiates with pharmaceutical companies to set a price for the drug, using methods such as benchmarking against prices in other countries, assessing clinical value, and considering production costs. The NHSA also leads volume-based procurement (VBPs) for drugs with a well-established clinical profile, aiming to reduce prices through economies of scale.
Additionally, the two-invoice system, introduced in 2016, improves transparency and reduces prices by requiring pharmaceutical manufacturers to issue invoices to distributors and distributors to issue invoices to medical institutions. As a result, the average percentage of price reduction for drugs included in the NRDL has been around 50% since 2016, putting pressure on pharmaceutical companies to maintain profitability while remaining competitive in the market. The mechanism also encourages market competition and value-based pricing, with the government considering value-based pricing for off-patent originators. Overall, China's reimbursement mechanism plays a crucial role in shaping the pricing of pharmaceutical products, ensuring that prices are reasonable and fair while balancing accessibility and affordability.
Competitive Landscape
Key Players
Here are some of the major key players in the China Financial Assistance Programs Market:
- CSPC Pharmaceuticals
- Cardinal Health
- Sinopharm Group Co Ltd
- Roche
- Pfizer
- Bayer
- Sanofi
- Novartis
- Merck
- GSK
1. Executive Summary
1.1 Service Overview
1.2 Global Scenario
1.3 Country Overview
1.4 Healthcare Scenario in Country
1.5 Healthcare Services Market in Country
1.6 Recent Developments in the Country
2. Market Size and Forecasting
2.1 Market Size (With Excel and Methodology)
2.2 Market Segmentation (Check all Segments in Segmentation Section)
3. Market Dynamics
3.1 Market Drivers
3.2 Market Restraints
4. Competitive Landscape
4.1 Major Market Share
4.2 Key Company Profile (Check all Companies in the Summary Section)
4.2.1 Company
4.2.1.1 Overview
4.2.1.2 Product Applications and Services
4.2.1.3 Recent Developments
4.2.1.4 Partnerships Ecosystem
4.2.1.5 Financials (Based on Availability)
5. Reimbursement Scenario
5.1 Reimbursement Regulation
5.2 Reimbursement Process for Services
5.3 Reimbursement Process for Treatment
6. Methodology and Scope
China Financial Assistance Programs Market Segmentation
By Application
- Population Health Management
- Outpatient Health Management
- In-patient Health Management
- Others
By Therapeutics Area
- Health & Wellness
- Chronic Disease Management
- Other therapeutic area
By End Users
- Payers
- Providers
- Others
Methodology for Database Creation
Our database offers a comprehensive list of healthcare centers, meticulously curated to provide detailed information on a wide range of specialties and services. It includes top-tier hospitals, clinics, and diagnostic facilities across 30 countries and 24 specialties, ensuring users can find the healthcare services they need.
Additionally, we provide a comprehensive list of Key Opinion Leaders (KOLs) based on your requirements. Our curated list captures various crucial aspects of the KOLs, offering more than just general information. Whether you're looking to boost brand awareness, drive engagement, or launch a new product, our extensive list of KOLs ensures you have the right experts by your side. Covering 30 countries and 36 specialties, our database guarantees access to the best KOLs in the healthcare industry, supporting strategic decisions and enhancing your initiatives.
How Do We Get It?
Our database is created and maintained through a combination of secondary and primary research methodologies.
1. Secondary Research
With many years of experience in the healthcare field, we have our own rich proprietary data from various past projects. This historical data serves as the foundation for our database. Our continuous process of gathering data involves:
- Analyzing historical proprietary data collected from multiple projects.
- Regularly updating our existing data sets with new findings and trends.
- Ensuring data consistency and accuracy through rigorous validation processes.
With extensive experience in the field, we have developed a proprietary GenAI-based technology that is uniquely tailored to our organization. This advanced technology enables us to scan a wide array of relevant information sources across the internet. Our data-gathering process includes:
- Searching through academic conferences, published research, citations, and social media platforms
- Collecting and compiling diverse data to build a comprehensive and detailed database
- Continuously updating our database with new information to ensure its relevance and accuracy
2. Primary Research
To complement and validate our secondary data, we engage in primary research through local tie-ups and partnerships. This process involves:
- Collaborating with local healthcare providers, hospitals, and clinics to gather real-time data.
- Conducting surveys, interviews, and field studies to collect fresh data directly from the source.
- Continuously refreshing our database to ensure that the information remains current and reliable.
- Validating secondary data through cross-referencing with primary data to ensure accuracy and relevance.
Combining Secondary and Primary Research
By integrating both secondary and primary research methodologies, we ensure that our database is comprehensive, accurate, and up-to-date. The combined process involves:
- Merging historical data from secondary research with real-time data from primary research.
- Conducting thorough data validation and cleansing to remove inconsistencies and errors.
- Organizing data into a structured format that is easily accessible and usable for various applications.
- Continuously monitoring and updating the database to reflect the latest developments and trends in the healthcare field.
Through this meticulous process, we create a final database tailored to each region and domain within the healthcare industry. This approach ensures that our clients receive reliable and relevant data, empowering them to make informed decisions and drive innovation in their respective fields.
To request a free sample copy of this report, please complete the form below.
We value your inquiry and offer free customization with every report to fulfil your exact research needs.








































