Canada Multiple Myeloma Therapeutics Market Analysis
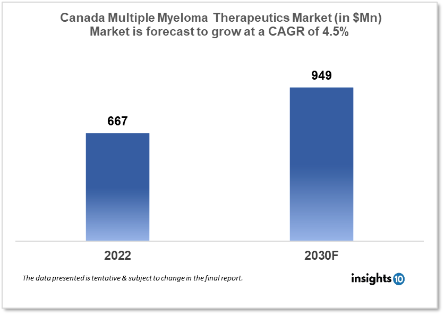
Canada's Multiple Myeloma Therapeutics Market was valued at $667 Mn in 2022 and is estimated to expand at a CAGR of 4.5% from 2022 to 2030 and will reach $849 Mn in 2030. One of the main reasons propelling the growth of this Market is the increasing adoption of combination therapies and technological advancements. The Market is segmented by type, drug and distribution channel. Some key players in this market are Apobiologix, Knight Therapeutics., Medexus Pharmaceuticals, Therapure Biopharma, Bloom Burton & Co., and others.
Buy Now

Canada Multiple Myeloma Therapeutics Market Executive Summary
Canada's Multiple Myeloma Therapeutics Market was valued at $667 Mn in 2022 and is estimated to expand at a CAGR of 4.5% from 2022 to 2030 and will reach $849 Mn in 2030. Multiple myeloma, also known as Kahler's disease, is a type of blood cancer that mostly affects plasma cells. Chemotherapeutic medicines, corticosteroids, and immunomodulatory medications are among the most frequent types of multiple myeloma drugs. These medications promote bone healing, avoid hypercalcemia, bone fracture, spinal cord compression, and anaemia, and reduce the need for chemotherapy. Several anthracycline antibiotics and alkylating drugs, such as melphalan, doxorubicin, vincristine, and liposomal doxorubicin, are used as chemotherapy medicines. Proteasome inhibitors, such as bortezomib, and other substances, such as dexamethasone, prednisone, and thalidomide, are among the targeted therapy medications. One of the primary reasons driving market expansion is significant improvements in the healthcare industry, as well as the rising prevalence of haematological cancer.
Market Dynamics
Market Growth Drivers
There have been significant advancements in the development of new therapies for multiple myeloma in recent years, including immunomodulatory drugs, proteasome inhibitors, and monoclonal antibodies. These new therapies offer better efficacy and safety profiles compared to traditional chemotherapy, which is driving demand for these treatments. Combination therapies, which involve the use of two or more drugs to treat multiple myeloma, are becoming increasingly popular. These therapies have been shown to improve patient outcomes and reduce the risk of disease progression. As a result, the adoption of combination therapies is driving market growth. The aging population is at a higher risk of developing multiple myeloma, as the incidence of the disease increases with age. As the population ages, the demand for multiple myeloma therapeutics is expected to increase. Technological advancements, such as the development of new diagnostic tools and targeted therapies, are driving growth in the multiple myeloma therapeutics market. These advancements are enabling earlier diagnosis and more effective treatment of the disease.
Market Restraints
he cost of multiple myeloma treatment can be high, particularly for newer therapies. This can create financial burdens for patients and healthcare systems, and limit access to treatment. Although new therapies are being developed, they may not be widely available to patients due to factors such as cost, limited production capacity, and slow regulatory approval processes. Reimbursement for multiple myeloma treatments can be challenging, particularly for newer therapies that are not yet covered by insurance plans. This can create barriers to access for patients who cannot afford the high out-of-pocket costs. Multiple myeloma therapies can cause significant side effects, including fatigue, nausea, and neuropathy. These side effects can impact patient quality of life and limit treatment adherence. Alternative treatments, such as stem cell transplantation, may compete with drug therapies for multiple myeloma. While drug therapies are often preferred due to their ease of administration and lower risks, alternative treatments may be preferred by some patients or physicians.
Competitive Landscape
Key Players
- Apobiologix.
- Knight Therapeutics.
- Medexus Pharmaceuticals
- Therapure Biopharma
- Bloom Burton & Co.
- Bristol Myers Squibb Company
- Amgen
- Johnson & Johnson Services
- AbbVie
Healthcare Policies and Regulatory Landscape
The healthcare policy and regulatory framework for the multiple myeloma therapeutics market in Canada is complex and is governed by several bodies, including Health Canada, the Canadian Agency for Drugs and Technologies in Health (CADTH), and the pan-Canadian Oncology Drug Review (pCODR). Health Canada is responsible for regulating drugs and medical devices in Canada. The agency reviews and approves new drugs before they can be marketed in the country. Health Canada also oversees post-market surveillance of drugs to ensure their safety and effectiveness.
CADTH is a non-profit organization that provides evidence-based assessments of the clinical and economic value of new drugs and medical technologies. Its assessments are used by Canadian health authorities and public payers to inform their reimbursement decisions.
pCODR is a partnership between Canadian provinces and territories to evaluate the clinical and cost-effectiveness of oncology drugs. The agency provides recommendations to public payers on whether to fund new cancer therapies based on their clinical and economic value.
Reimbursement Scenario
The reimbursement scenario for multiple myeloma therapeutics in Canada varies depending on the province or territory in which a patient is receiving treatment. In general, reimbursement for cancer drugs is provided through publicly funded drug plans and private insurance plans.
Public drug plans in Canada typically cover the cost of cancer drugs for patients who meet certain eligibility criteria, such as having a valid provincial health card and a prescription from a licensed physician. However, the extent of coverage and reimbursement rates may vary by drug, province, and patient population. Private insurance plans may also cover the cost of cancer drugs, although the extent of coverage and reimbursement rates may vary depending on the specific plan. In recent years, the Canadian government has taken steps to improve access to cancer therapies, including the introduction of the pan-Canadian Pharmaceutical Alliance (pCPA), which negotiates drug prices on behalf of public payers, and the creation of the Canadian Drug Agency (CDA), which is intended to streamline drug evaluation and reimbursement processes.
1. Executive Summary
1.1 Disease Overview
1.2 Global Scenario
1.3 Country Overview
1.4 Healthcare Scenario in Country
1.5 Patient Journey
1.6 Health Insurance Coverage in Country
1.7 Active Pharmaceutical Ingredient (API)
1.8 Recent Developments in the Country
2. Market Size and Forecasting
2.1 Epidemiology of Disease
2.2 Market Size (With Excel & Methodology)
2.3 Market Segmentation (Check all Segments in Segmentation Section)
3. Market Dynamics
3.1 Market Drivers
3.2 Market Restraints
4. Competitive Landscape
4.1 Major Market Share
4.2 Key Company Profile (Check all Companies in the Summary Section)
4.2.1 Company
4.2.1.1 Overview
4.2.1.2 Product Applications and Services
4.2.1.3 Recent Developments
4.2.1.4 Partnerships Ecosystem
4.2.1.5 Financials (Based on Availability)
5. Reimbursement Scenario
5.1 Reimbursement Regulation
5.2 Reimbursement Process for Diagnosis
5.3 Reimbursement Process for Treatment
6. Methodology and Scope
Multiple Myeloma Therapeutics Market Segmentation
By Treatment
- Chemotherapy
- Immunotherapy
- Targeted therapy
- Radiation therapy
- Stem cell transplant
By Distribution Channel
- Hospitals
- Retail
- Online
By End User (Revenue, USD Bn):
- Hospitals
- Clinics
- Cancer Research Centers
By Drug Class
Immunomodulatory drugs (IMiDs)
One of the most common therapies used to treat myeloma are immunomodulatory drugs, or IMiDs. These drugs work by modifying the immune system to attack myeloma cells and have been a significant advance in the treatment of multiple myeloma. Some of the commonly used IMiDs in multiple myeloma include:
- Lenalidomide (Revlimid): Lenalidomide is an oral medication that is used in the treatment of multiple myeloma, as well as other blood cancers such as myelodysplastic syndromes (MDS). It may help the immune system in eliminating cancerous or abnormal blood cells. Moreover, it might stop the development of new blood vessels that tumours require to expand.
- Pomalidomide (Pomalyst): Pomalidomide is an oral medication that is used to treat multiple myeloma. It works in a similar way to lenalidomide, by enhancing the immune system's ability to target cancer cells. Also, it makes it easier for immune cells to eliminate faulty myeloma cells, aiding in the production of healthy blood cells in the myeloma.
- Thalidomide (Thalomid): Thalidomide was the first IMiD to be used in the treatment of multiple myeloma. It works by modulating the immune system and preventing the growth of blood vessels that supply the tumor
- CC- 4047 (Actimid): CC-4047 is a newer IMiD that is still under investigation for the treatment of multiple myeloma. It works by inhibiting the growth of cancer cells and promoting their death.
Proteasome inhibitors
Proteasome inhibitors are a class of drugs that are commonly used in the treatment of multiple myeloma. They work by blocking the activity of proteasomes, which are cellular structures that break down proteins. This leads to the accumulation of proteins within the myeloma cells, ultimately causing their death. Some proteasome inhibitors used in multiple myeloma include:
- Bortezomib (Velcade): Bortezomib was the first proteasome inhibitor approved for the treatment of multiple myeloma. It is given by injection and is often used in combination with other drugs, such as chemotherapy or immunomodulatory drugs. Bortezomib is highly effective in inducing remissions in newly diagnosed and relapsed/refractory multiple myeloma patients.
- Carfilzomib (Kyprolis): Carfilzomib is a newer proteasome inhibitor that is approved for the treatment of multiple myeloma. It is given by injection and can be used as a single agent or in combination with other drugs. Carfilzomib has shown excellent results in heavily pretreated patients with relapsed/refractory multiple myeloma.
- Ixazomib (Ninlaro): Ixazomib is an oral proteasome inhibitor that is approved for use in combination with lenalidomide and dexamethasone for the treatment of multiple myeloma. It is the first oral proteasome inhibitor and offers the convenience of home administration.
Monoclonal antibodies:
Monoclonal antibodies, target specific proteins on the surface of myeloma cells, causing them to be destroyed by the immune system. Some of the commonly used monoclonal antibodies in multiple myeloma include:
- Daratumumab (Darzalex): Daratumumab is a monoclonal antibody that targets a protein called CD38, which is highly expressed on the surface of myeloma cells. By binding to CD38, daratumumab triggers the immune system to attack and destroy the cancer cells. It is approved for use in multiple myeloma in combination with other drugs, such as lenalidomide or bortezomib.
- Elotuzumab (Empliciti): Elotuzumab is a monoclonal antibody that targets a protein called SLAMF7, which is also expressed on the surface of myeloma cells. By binding to SLAMF7, elotuzumab enhances the immune system's ability to attack the cancer cells. It is approved for use in combination with lenalidomide and dexamethasone for the treatment of multiple myeloma.
- Isatuximab (Sarclisa): Isatuximab is a monoclonal antibody that targets a protein called CD38, similar to daratumumab. By binding to CD38, isatuximab triggers the immune system to attack and destroy the cancer cells. It is approved for use in combination with pomalidomide and dexamethasone for the treatment of multiple myeloma.
Chemotherapy drugs
Chemotherapy drugs work by killing rapidly dividing cells, including cancer cells. Chemotherapy is often used in combination with other drugs, such as steroids, immunomodulatory drugs, or proteasome inhibitors, to improve their effectiveness. Here are some chemotherapy drugs used in multiple myeloma:
- Melphalan: Melphalan is an alkylating agent that is commonly used in the treatment of multiple myeloma. It is used as a preventative measure before having a stem cell transplant to treat multiple myeloma. It works by damaging the DNA of cancer cells, leading to their death. Melphalan is often used in combination with other drugs, such as prednisone, to treat newly diagnosed multiple myeloma.
- Cyclophosphamide: Cyclophosphamide works by damaging the DNA of cancer cells, leading to their death. Cyclophosphamide is often used in combination with other drugs, such as dexamethasone, to treat relapsed or refractory multiple myeloma. Cyclophosphamide inhibits cancer cell proliferation, causing the body to kill the cancer cells.
- Doxorubicin: Doxorubicin works by inhibiting the synthesis of DNA and RNA, leading to the death of cancer cells. Doxorubicin is often used in combination with other drugs, such as bortezomib or dexamethasone, to treat newly diagnosed or relapsed/refractory multiple myeloma. Doxorubicin belongs to the anthracycline class of chemotherapeutic drugs, which also includes daunorubicin, idarubicin, and epirubicin.
- Etoposide: Etoposide is a topoisomerase inhibitor chemotherapy drug that is used in the treatment of multiple myeloma. It works by inhibiting the activity of topoisomerase enzymes, which are necessary for DNA replication and repair. Etoposide is often used in combination with other drugs, such as cisplatin, to treat relapsed or refractory multiple myeloma. It works by reducing or preventing cancer cell proliferation in your body.
Steroids
Steroids such as dexamethasone and prednisone are often used in combination with other drugs to treat multiple myeloma. They can reduce inflammation, suppress the immune system, and promote the death of myeloma cells.
- Dexamethasone: Dexamethasone works by reducing inflammation and suppressing the immune system. Dexamethasone is often used in combination with other drugs to treat relapsed or refractory multiple myeloma.
- Prednisone: Prednisone works by suppressing the immune system and reducing inflammation. Prednisone is often used in combination with other drugs, such as chemotherapy, to treat newly diagnosed multiple myeloma.
- Methylprednisolone: Methylprednisolone is a steroid that is similar to prednisone and is also used in the treatment of multiple myeloma. It works by suppressing the immune system and reducing inflammation. Methylprednisolone is often used in combination with other drugs to treat relapsed or refractory multiple myeloma.
Steroids are effective in reducing inflammation and suppressing the immune system, which can help to control the growth of myeloma cells. However, they can have side effects, such as weight gain, mood changes, and increased risk of infection, so their use needs to be carefully monitored.
Others
Other drug classes used to treat multiple myeloma include:
- Histone deacetylase inhibitors- A new class of cytostatic drugs that suppress tumour cell proliferation in vitro and in vivo by inducing cell cycle arrest, differentiation, and/or apoptosis
- Immune checkpoint inhibitors- Checkpoint proteins are produced by some immune system cells, such as T cells, as well as some cancer cells. These checkpoints prevent too aggressive immune responses and, in some cases, prevent T cells from destroying cancer cells.
- Targeted therapies- Proteasome inhibitors are one type of targeted therapy for multiple myeloma. Proteasome inhibitors include bortezomib (Velcade), carfilzomib (Kyprolis), and ixazomib (Ninlaro). They target proteasomes, which are enzymes that breakdown proteins in cells.
Methodology for Database Creation
Our database offers a comprehensive list of healthcare centers, meticulously curated to provide detailed information on a wide range of specialties and services. It includes top-tier hospitals, clinics, and diagnostic facilities across 30 countries and 24 specialties, ensuring users can find the healthcare services they need.
Additionally, we provide a comprehensive list of Key Opinion Leaders (KOLs) based on your requirements. Our curated list captures various crucial aspects of the KOLs, offering more than just general information. Whether you're looking to boost brand awareness, drive engagement, or launch a new product, our extensive list of KOLs ensures you have the right experts by your side. Covering 30 countries and 36 specialties, our database guarantees access to the best KOLs in the healthcare industry, supporting strategic decisions and enhancing your initiatives.
How Do We Get It?
Our database is created and maintained through a combination of secondary and primary research methodologies.
1. Secondary Research
With many years of experience in the healthcare field, we have our own rich proprietary data from various past projects. This historical data serves as the foundation for our database. Our continuous process of gathering data involves:
- Analyzing historical proprietary data collected from multiple projects.
- Regularly updating our existing data sets with new findings and trends.
- Ensuring data consistency and accuracy through rigorous validation processes.
With extensive experience in the field, we have developed a proprietary GenAI-based technology that is uniquely tailored to our organization. This advanced technology enables us to scan a wide array of relevant information sources across the internet. Our data-gathering process includes:
- Searching through academic conferences, published research, citations, and social media platforms
- Collecting and compiling diverse data to build a comprehensive and detailed database
- Continuously updating our database with new information to ensure its relevance and accuracy
2. Primary Research
To complement and validate our secondary data, we engage in primary research through local tie-ups and partnerships. This process involves:
- Collaborating with local healthcare providers, hospitals, and clinics to gather real-time data.
- Conducting surveys, interviews, and field studies to collect fresh data directly from the source.
- Continuously refreshing our database to ensure that the information remains current and reliable.
- Validating secondary data through cross-referencing with primary data to ensure accuracy and relevance.
Combining Secondary and Primary Research
By integrating both secondary and primary research methodologies, we ensure that our database is comprehensive, accurate, and up-to-date. The combined process involves:
- Merging historical data from secondary research with real-time data from primary research.
- Conducting thorough data validation and cleansing to remove inconsistencies and errors.
- Organizing data into a structured format that is easily accessible and usable for various applications.
- Continuously monitoring and updating the database to reflect the latest developments and trends in the healthcare field.
Through this meticulous process, we create a final database tailored to each region and domain within the healthcare industry. This approach ensures that our clients receive reliable and relevant data, empowering them to make informed decisions and drive innovation in their respective fields.
To request a free sample copy of this report, please complete the form below.
We value your inquiry and offer free customization with every report to fulfil your exact research needs.








































