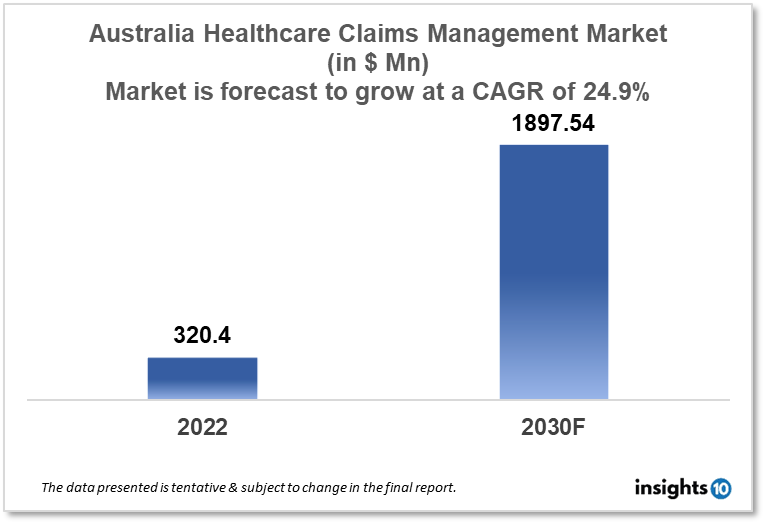
Australia Healthcare Claims Management Market Analysis
The Australian healthcare claims management market is projected to grow from $320.4 Mn in 2022 to $1897.54 Mn by 2030, registering a CAGR of 24.9% during the forecast period of 2022 - 2030. The main factors driving the growth would be an increase in healthcare provider consolidation, technological advancements, regulatory changes and an increase in healthcare spending. The market is segmented by component, type, by delivery mode and end-user. Some of the major players include Proclaim, Medibank, Riskware, Cognizant and Accenture.
Buy Now

Australia Healthcare Claims Management Market Executive Summary
The Australian healthcare claims management market is projected to grow from $320.4 Mn in 2022 to $1897.54 Mn by 2030, registering a CAGR of 24.9% during the forecast period of 2022 - 2030. In Australia, healthcare costs were $202.5 Bn, or $7,926 per person, in 2019–20. Compared to the decade average of 3.4%, the actual increase in healthcare spending was lower at 1.8%. In Australia, the government covers the majority of the cost of healthcare, but patients also foot a sizable percentage of the bill.
Healthcare providers in Australia can handle the process of getting paid by health insurance companies with the aid of the quickly expanding sector of healthcare claims management. Healthcare providers may file and handle claims more effectively, with fewer errors and better overall revenue cycle management, due to the technology solutions and services offered by healthcare claims management firms.
There is a greater need for more streamlined and effective claims management systems due to the rising demand for healthcare services in Australia, the rising number of health insurance claims, and the complexity of the claims process. In Australia, systems for managing healthcare claims frequently involve computerised claim processing, patient eligibility checking, payment processing, and rejection management. These solutions can be tailored to the unique requirements of healthcare organisations, such as hospitals, clinics, and medical practices.
Market Dynamics
Market Growth Drivers
The Australian healthcare claims management market is expected to be driven by factors such as:
- Increase in healthcare provider consolidation- Larger healthcare organisations are acquiring smaller ones as provider consolidation in the Australian healthcare sector increases. As a result, more claims are being processed, which has increased the demand for more effective claims management solutions
- Technological advancements- Several components of the claims management process are now able to be automated by technological developments like cloud computing and artificial intelligence. The efficiency and precision of the process have increased, which has helped the market for healthcare claims management expand
- Regulatory changes- In Australia, the healthcare sector is extensively regulated, and the reimbursement process is governed by a number of rules and regulations. Regulations like the Medicare Benefits Schedule and the Health Insurance Act of 1973 have enhanced the demand for effective claims management solutions
- Increase in healthcare spending- The demand for healthcare services has increased as a result of the Australian government's increased healthcare spending. The demand for healthcare claims management solutions has increased as a result of the increase in claims made by healthcare providers
Market Restraints
The following factors are expected to limit the growth of the healthcare claims management market in Australia:
- Restricted system interoperability- Medical billing and claims management software frequently needs to interact with other software, such as electronic health records and billing software. It may be challenging to properly adopt and use healthcare claims management solutions due to the lack of interoperability across various systems
- Data privacy and security concerns- In Australia, there are stringent laws governing data privacy and security in the healthcare sector. Healthcare claims management businesses must make sure that patient data is secure and complies with laws such as the My Health Records Act of 2012 and the Privacy Act of 1988
- Opposition to change- Many healthcare professionals could be reluctant to use new technological solutions, preferring to continue with their manual or antiquated procedures instead. The adoption of healthcare claims management solutions may be constrained as a result
- Cost issues- The expense of deployment and continuing maintenance may deter healthcare providers from investing in healthcare claims management technologies. This may prevent certain healthcare organisations, especially those with lesser resources, from adopting these solutions
Competitive Landscape
Key Players
- Proclaim (AUS)- a tech-savvy expert claim manager that goes above and above to offer creative outsourced claim management. It offers solutions for all types of general insurance policies, including those for professional indemnity, public and product liability, property, auto, accident and health, and other specialty lines
- Medibank (AUS)- uses Civica’s digital platform and offers a better user experience with quicker transaction completion times and rapid claim determinations. Additionally, it permits fund organisations to speak with members directly while making the claim and provides more security via tokens and encryption
- Riskware (AUS)- based in Melbourne, offers various products and services including claims management. It provides cutting-edge case management tools, great transparency, powerful return-to-work and rehabilitation features, and mechanisms for managing compensation
- Cognizant- an international company that offers solutions for processing medical claims, and operational, digital, and consulting services. The primary technical areas that are transforming business include the cloud, IoT, AI, and software engineering
- Accenture- a multinational professional services firm that offers clients in Australia and other nations services for managing medical claims. Customer support, fraud and abuse detection, analytics and reporting, as well as claims processing and management, are all included in Accenture's healthcare management services
Notable Deals
September 2020: With the help of the collaboration between Civica, Medibank, and LanternPay, private health insurance claims were transformed. Through this collaboration, the new cloud solution gives Medibank clients a better user experience, faster transaction funding, and instant claim judgements. Additionally, it permits fund organisations to speak with members directly while making the claim and provides more security via tokens and encryption.
1. Executive Summary
1.1 Service Overview
1.2 Global Scenario
1.3 Country Overview
1.4 Healthcare Scenario in Country
1.5 Healthcare Services Market in Country
1.6 Recent Developments in the Country
2. Market Size and Forecasting
2.1 Market Size (With Excel and Methodology)
2.2 Market Segmentation (Check all Segments in Segmentation Section)
3. Market Dynamics
3.1 Market Drivers
3.2 Market Restraints
4. Competitive Landscape
4.1 Major Market Share
4.2 Key Company Profile (Check all Companies in the Summary Section)
4.2.1 Company
4.2.1.1 Overview
4.2.1.2 Product Applications and Services
4.2.1.3 Recent Developments
4.2.1.4 Partnerships Ecosystem
4.2.1.5 Financials (Based on Availability)
5. Reimbursement Scenario
5.1 Reimbursement Regulation
5.2 Reimbursement Process for Services
5.3 Reimbursement Process for Treatment
6. Methodology and Scope
Healthcare Claims Management Market Segmentation
By Component (Revenue, USD Billion):
Further breakdown of the software and services segment of the healthcare claims management market
- Software
- Services
By Type (Revenue, USD Billion):
Although they have nothing to do with it, skills unrelated to patient care are equally crucial for any healthcare organization that wants to stay in business. Among these are managing intricate insurance regulations, comprehending best practices for data collection, and analyzing data to identify areas for development. For the above reasons, providers are constantly looking for methods to improve claim administration and medical billing systems. Setting up an integrated billing and claims processing system is one approach to accomplish this, which has a number of benefits.
- Integrated Solutions
- Standalone Solutions
By Delivery Mode (Revenue, USD Billion):
- On-Premise
- Cloud-Based
By End User (Revenue, USD Billion):
- Healthcare Payers
- Healthcare Providers
- Other End Users
Healthcare payers in this market are anticipated to rise quickly over the course of the projection period because of the installation of strict regulatory requirements, a lack of experienced personnel internally for claims processing, rising healthcare expenditures, and fraud associated with those charges. Payers have also assisted healthcare providers by creating a web-based and cloud-based interface that helps them manage medical billing and associated claims and offers accurate and timely information about the epidemic.
Methodology for Database Creation
Our database offers a comprehensive list of healthcare centers, meticulously curated to provide detailed information on a wide range of specialties and services. It includes top-tier hospitals, clinics, and diagnostic facilities across 30 countries and 24 specialties, ensuring users can find the healthcare services they need.
Additionally, we provide a comprehensive list of Key Opinion Leaders (KOLs) based on your requirements. Our curated list captures various crucial aspects of the KOLs, offering more than just general information. Whether you're looking to boost brand awareness, drive engagement, or launch a new product, our extensive list of KOLs ensures you have the right experts by your side. Covering 30 countries and 36 specialties, our database guarantees access to the best KOLs in the healthcare industry, supporting strategic decisions and enhancing your initiatives.
How Do We Get It?
Our database is created and maintained through a combination of secondary and primary research methodologies.
1. Secondary Research
With many years of experience in the healthcare field, we have our own rich proprietary data from various past projects. This historical data serves as the foundation for our database. Our continuous process of gathering data involves:
- Analyzing historical proprietary data collected from multiple projects.
- Regularly updating our existing data sets with new findings and trends.
- Ensuring data consistency and accuracy through rigorous validation processes.
With extensive experience in the field, we have developed a proprietary GenAI-based technology that is uniquely tailored to our organization. This advanced technology enables us to scan a wide array of relevant information sources across the internet. Our data-gathering process includes:
- Searching through academic conferences, published research, citations, and social media platforms
- Collecting and compiling diverse data to build a comprehensive and detailed database
- Continuously updating our database with new information to ensure its relevance and accuracy
2. Primary Research
To complement and validate our secondary data, we engage in primary research through local tie-ups and partnerships. This process involves:
- Collaborating with local healthcare providers, hospitals, and clinics to gather real-time data.
- Conducting surveys, interviews, and field studies to collect fresh data directly from the source.
- Continuously refreshing our database to ensure that the information remains current and reliable.
- Validating secondary data through cross-referencing with primary data to ensure accuracy and relevance.
Combining Secondary and Primary Research
By integrating both secondary and primary research methodologies, we ensure that our database is comprehensive, accurate, and up-to-date. The combined process involves:
- Merging historical data from secondary research with real-time data from primary research.
- Conducting thorough data validation and cleansing to remove inconsistencies and errors.
- Organizing data into a structured format that is easily accessible and usable for various applications.
- Continuously monitoring and updating the database to reflect the latest developments and trends in the healthcare field.
Through this meticulous process, we create a final database tailored to each region and domain within the healthcare industry. This approach ensures that our clients receive reliable and relevant data, empowering them to make informed decisions and drive innovation in their respective fields.
To request a free sample copy of this report, please complete the form below.
We value your inquiry and offer free customization with every report to fulfil your exact research needs.